Views from RCM leaders
For the first time in several years, hospital and health system executives are expressing optimism about their financial future – but with some very clear caveats. We recently sat down with four C-suite leaders to get their take on the complex process of billing and reimbursement, and how providers and payers are clashing over the validity and value of claims.
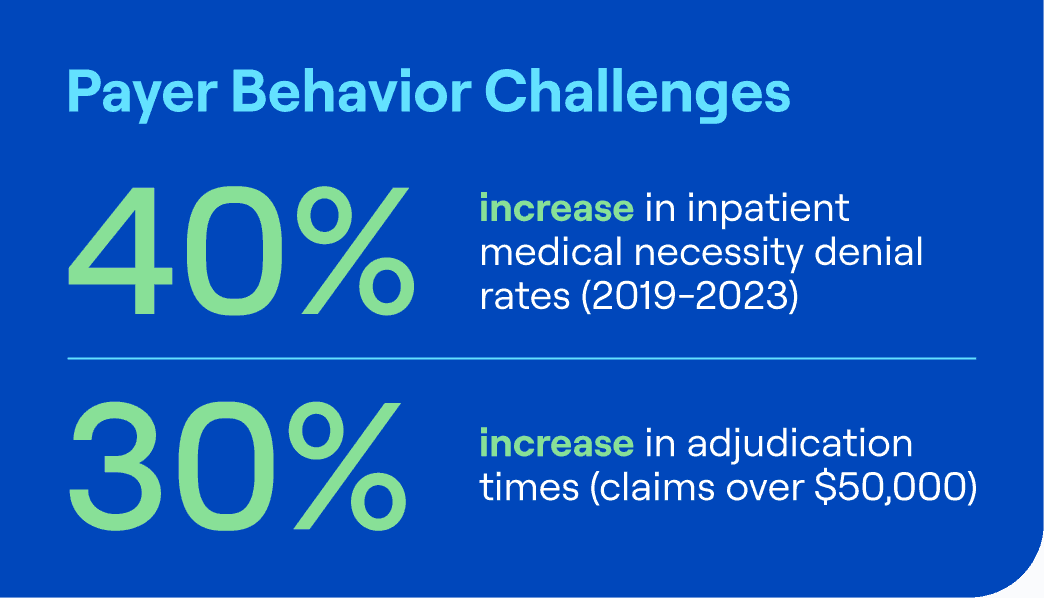
Our work with 95 of the top 100 health systems in the country gives us a unique view into millions of transactions covering more than $850 billion in net patient revenue (NPR). Our data shows a 40% increase in medical necessity denial rates for inpatient claims from 2019 to 2023, and a 30% increase in adjudication times for high dollar claims over $50,000.
This means providers are spending more time and money on administrative tasks such as appealing denials, resubmitting claims and collecting payments instead of focusing on patient care. Moreover, denials create frustration and anxiety for patients, who may face unexpected bills or delays in accessing care.
To cope with the challenge of denials, providers are adopting various strategies, ranging from collaborative to confrontational:
1. Building constructive relationships with payers
Some providers are trying to establish trust and rapport with payers, especially at the physician level, to facilitate communication and negotiation.
2. Using artificial intelligence to automate and optimize claims
Some providers are investing in technology solutions that can help them reduce errors, improve documentation and streamline workflows. However, some are skeptical about the potential of AI, as it may also be used by payers to deny claims more efficiently.
3. Diversifying revenue sources by launching or partnering with provider-owned health plans
Some providers are trying to bypass the traditional payer-provider relationship by becoming payers themselves or by collaborating with other providers who have their own health plans. This way, they can have more control and flexibility over the reimbursement process and the quality of care.
Expert perspectives
One of the challenges that providers face in dealing with denials is the increasing use of data analytics by payers, who often deny claims based on how they are billed, rather than on the merits of the case. Sarah Mendiola, VP Retrospective Services, Clinical, Coding and Complex Denials at R1 RCM, believes that AI and bots can be helpful tools for providers, but they need to be used intelligently and strategically. She suggests that AI can be more effective in preventing denials by automating tasks such as eligibility verification, authorization confirmation, and benefit checking.
Mendiola also sees potential for AI to assist in appealing denials by summarizing medical records and arguments, but she cautions that “clinical knowledge and expertise are still essential to make a strong case”. Therefore, she advocates for a balanced approach that combines technology and human skills to optimize the denial management process.
“Payer and Provider relationships are at an all-time level of frustration,” according to Shawn Stack, Director of Perspectives and Analysis at HFMA. “I am fielding calls from providers and consultants weekly seeking advice on how to appropriately terminate managed care contracts due to unreconcilable differences, the main concern of those calling me are to make certain the patient’s continuity of care is not jeopardized and to gain clearer understanding of the protections that Federal Transparency and the No Surprises Act regulations offer in these scenarios.”
Stack added, “There are no winners in these contentious relationships and there will be a breaking point when federal and state oversight will need to step in and act, if we continue to fail to collaborate with each other in the best interest of our patients and communities.”
Opportunities to improve
Denials are a major pain point for US healthcare providers, as they affect their financial performance, operational efficiency, and patient satisfaction. To address this problem, providers need to adopt a proactive and holistic approach that involves improving their internal processes, engaging with payers, leveraging technology, and exploring new business models. By doing so, they can reduce the administrative burden and cost of denials and focus more on delivering high-quality and affordable care to their patients.
If you’d like to read more about how we are helping providers across the country tackle this issue, read our new eBook: Mastering Denials Management.