2020 is beginning to wind down, but COVID-19’s financial impact on physician practices isn’t. As The Washington Post recently stated, “many of the doctors…who form the backbone of front-line care are barely hanging on,” and for primary care providers, “it’s an extinction-level event.”
The pandemic’s effect on the healthcare revenue cycle has given way to a number of terms such as “financial resilience” and “financial recovery.” While the wording may vary, these terms all point to the same key fact: To stay viable, physician practices must employ new revenue cycle strategies or find ways to strengthen existing ones.
Coding performance improvement falls into the latter category: all physician practices have coding processes, but not all coding processes are created alike. In a typical year, physician practices must adjust to thousands of coding changes; this year has brought myriad additional updates that address COVID-19 diagnoses and the expansion of telehealth. Having the right processes in place to ensure correct coding in the face of these potentially overwhelming changes can have a significant impact on a physician practice’s finances.
Coding Best Practices at Work: Optimizing HCC to Double Reimbursement
Best practices can optimize reimbursement through consistency in coding processes – creating standardization that helps ensure accuracy, completeness and expedience at every step. When R1 works with physician practices, we analyze their root causes of coding errors to help us determine where they can reap the greatest benefit through process improvement. A typical area that needs best practice processes is HCC (Hierarchical Condition Category) Coding.
A value-based rule that offers more funding for sicker patients, HCC coding assigns a score based on the patient’s number of symptoms. Within coding processes, knowing how to optimize HCC often has the largest impact on a practice’s overall performance. Besides ensuring accurate reimbursement, HCC optimization can also enable higher annual reimbursement limits from CMS. It can support higher Merit-Based Incentive Payment System (MIPS) scores and fewer payment reductions by increasing points for the cost of physician value calculations.
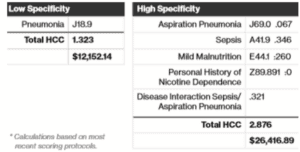
Below is an example of a physician coding a patient for pneumonia, which shows the impact of low specificity versus high specificity within HCC coding:
The total HCC score for the patient would be 1.323, which will result in a reimbursement of $12,152.14. Yet if the physician had been more specific, coding for “Aspiration Pneumonia, Sepsis, Mild Malnutrition, Personal History of Nicotine Dependence and Disease Interaction Sepsis/Aspiration Pneumonia,” the total HCC score more than doubles at 2.876 – yielding a reimbursement of $26,416.89. The higher specificity not only doubles the practice’s reimbursement, but also helps foster better clinical outcomes by giving clinicians a more accurate and comprehensive view of the patient’s health.
In addition to HCC optimization, physician practices can often leverage other best practices to achieve improvements that are less obvious but just as important. One example is analyzing coding for value-based care, which allows practices to identify new ways to compliantly optimize revenue from value-based contracts. As a result, practices frequently improve patient care as well as reimbursement.
Three Critical Best Practices for More Accurate and Complete Coding
Physician practices that consistently receive accurate and complete reimbursement while staying compliant typically employ coding best practices such as:
1. Be proactive about value-based care – Only about 50% of practices participate in any kind of value-based contract according to R1’s research, but a new report indicates COVID-19 will push the industry further away from fee-for-service (FFS). A recent Medical Economics article concurs, indicating the pandemic will lessen healthcare’s dependency on FFS and observing, “Practices in value-based programs appear to be better positioned to survive the COVID-19 crisis.”
Coupled with the many coding changes brought by COVID-19, adjusting for VBC can seem daunting. Develop a plan to help fully optimize your practice’s value-based reimbursement opportunities; for example, deploy best practice processes that support coding to the highest level of specificity. These processes will help your practice secure the more extensive and detailed data necessary for VBC.
2. Ramp up education about new legislation – Staying abreast of all legislation that impacts coding as well as the dates that regulatory changes take effect requires a formal and proactive coding education program. For example, earlier this year, Centers for Medicare and Medicaid Services (CMS) finalized add-on codes that will help providers more fully capture the resource costs of serving patients who require complex care. In January 2021, CMS will move from a points-based system to a medical necessity-based system for history, exam and medical decision making. A coding education program should ideally provide customized learning for clinicians and staff, providing information according to each person’s role in the coding process.
3. Make necessary changes in technology – While technology should be a tool to streamline and simplify processes, it can all too easily add complexity to the coding landscape. When healthcare moved to ICD-10 codes several years ago, even small practices estimated their transition costs would be upwards of $225,000. Practices that are challenged to stay abreast of new coding changes often cope with a high percentage of denials due to outdated codes. With constant coding changes, this perpetual state of transition requires significant resources that could otherwise be allocated to patient care. Make sure your RCM technology fosters speed and accuracy across all coding processes and supports best practices such as capturing and properly detailing all procedures to eliminate under-reporting.
Thriving in an era of unknowns
While physician practices are accustomed to healthcare’s ongoing evolution, the pandemic has accelerated the pace of change. Our care delivery model is irrevocably shifting and much remains unknown. At the same time, physician practices are trying to recover financially from a difficult if not crippling year. Maximizing every source of revenue is essential, and coding’s role in reimbursement cannot be overstated.
If maintaining up-to-date coding education and other best practices seems daunting, consider leveraging a trusted partner for part or all of the coding process. Look for a partner that can show how their processes and technology work together to support comprehensive coding best practices, and ask them to provide proven, metric-driven results. The right partner can help you conduct a root cause analysis, strengthen coding education, or even take on part or all of your coding workload.