- What We Do
- Back
- Enterprise Solutions
- Revenue Recovery
- Revenue Optimization
- Clinical Integrity
- Regulatory Navigation
- Who We Help
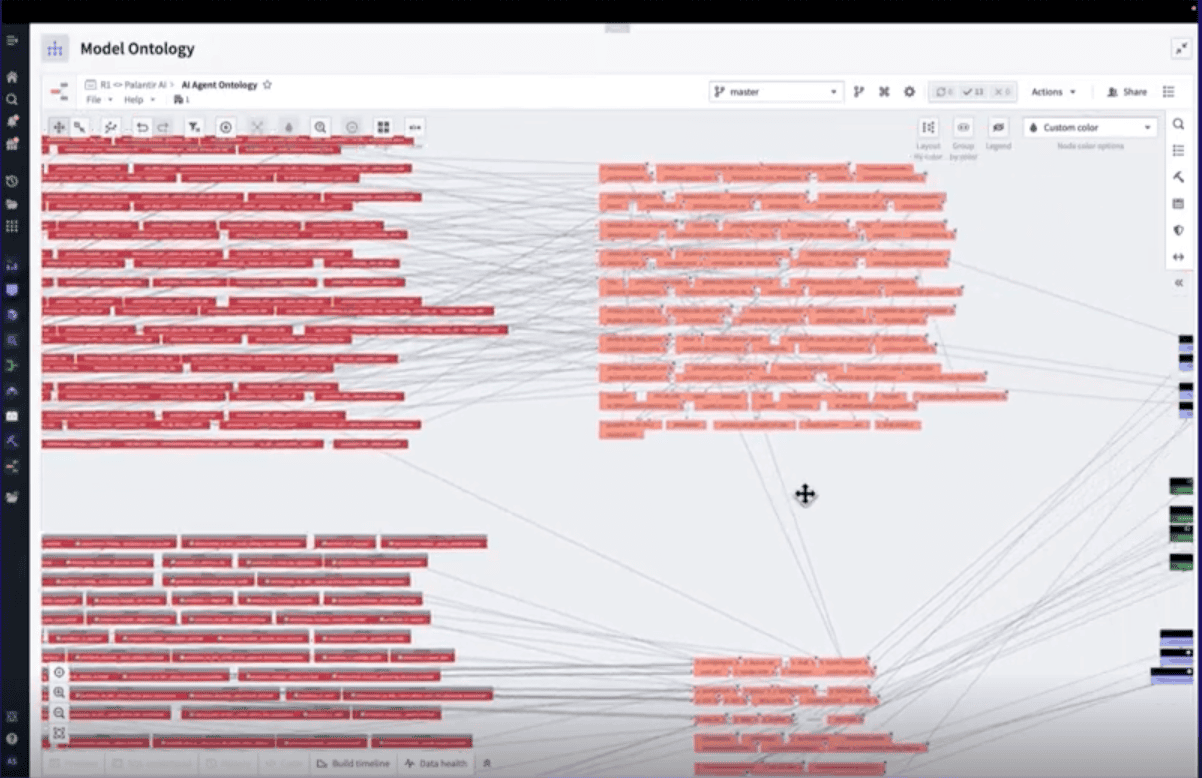
- Our Platform
- Insights and Resources
- About Us
- Careers
- Insights and Resources
- Articles
Articles
Subscribe to get the latest R1 resources in your inbox
Subscribe to our email list to get the latest in your inbox